This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 60 year old male patient, agriculture worker by profession, residents of Miryalguda, came to the OPD with chief complaints of:
Chief Complaints:
Loss of Power in left upper limb since 1 month
Loss of power in left lower limb since 4 days
Deviation of mouth towards right side since 4 days
History of Presenting Illness:
Patient was apparently asymptomatic 1 month ago, then he developed loss of power in left upper limb, sudden in onset, gradually progressive from distal to progressive direction.
Patient has used herbal medication for this.
Later he developed loss of power in left lower limb, 4 days ago, sudden in onset, gradually progressive in character.
He also developed deviation of mouth towards right side, 4 days ago which was sudden in onset, gradually progressive in character.
Past History:
History of loss of power in left upper limb , years ago which resolved after a couple of days.
History of tuberculosis, 3 years ago, took ATT medications for 6 months.
History of road traffic accident, 4 years ago, right wrist fracture and rod placed in right leg.
History of 2nd road traffic accident, 4 years ago, scapular fracture on the left side.
Patient was diagnosed with diabetes, used medications for a month then discontinued.
Not a known case of hypertension, coronary artery disease, epilepsy etc.
Personal History:
Mixed Diet (Veg, Non Veg)
Normal Bowel and bladder movements
Adequate sleep
Normal Appetite
Occasional Drinker (twice/month)
Smoked 1 bid-hi/day till a year ago.
Family History:
No one has similar complaints.
General Examination:
Pulse Rate: 63/minute
Respiratory Rate: 16/minute
Blood Pressure: 100/60 mmhg
SP02: 98*c
Pallor: Absent
Icterus: Absent
Clubbing: Absent
Cyanosis: Absent
Lymphadenopathy: Absent
Edema: Absent
Systemic Examination:
Cardiovascular System:
S1 sound heard
S2 sound heard
No murmurs heard
Respiratory System:
Vesicular Breath Sounds Heard
Trachea Position Central
No Dyspnoea
No wheeze
Abdomen:
Shape of Abdomen: Scaphoid
Tenderness: No
Palpable Mass: No
Hernial Orifices: Normal
Free fluid: No
Liver Palpable: No
Spleen Palpable: No
Bowel Sounds: Present
Central Nervous System:
Patient is conscious, coherent, co-operative
Speech: Slurred
General Examination:
Pulse Rate: 63/minute
Respiratory Rate: 16/minute
Blood Pressure: 100/60 mmhg
SP02: 98*c
Pallor: Absent
Icterus: Absent
Clubbing: Absent
Cyanosis: Absent
Lymphadenopathy: Absent
Edema: Absent
Systemic Examination:
Cardiovascular System:
S1 sound heard
S2 sound heard
No murmurs heard
Respiratory System:
Vesicular Breath Sounds Heard
Trachea Position Central
No Dyspnoea
No wheeze
Abdomen:
Shape of Abdomen: Scaphoid
Tenderness: No
Palpable Mass: No
Hernial Orifices: Normal
Free fluid: No
Liver Palpable: No
Spleen Palpable: No
Bowel Sounds: Present
Central Nervous System:
Patient is conscious, coherent, co-operative
Speech: Normal
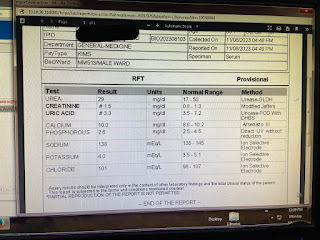
Investigations:
MRI Scan
Provisional Diagnosis:
Acute Ischemic Stroke
Treatment:
Tab. Ecosprin
Tab. MUT








Comments
Post a Comment